Note from the Product Coordinator: How to know if you’re eligible for the CCDS
by Karla Accorto
One of my favorite parts of working with ACDIS is getting to communicate with so many of you on a regular basis. If my name looks familiar—well, it could actually be for a lot of reasons, as I have trouble keeping my hands out of pretty much anything—but it’s likely because you’ve emailed info@acdis.org or acdis-inquiries@simplifycompliance.com and received a response from yours truly. I love hearing all of your thoughts, providing additional information, and generally getting the chance to connect with you.
This week, I wanted to chat about one of the questions I encounter most frequently: Am I eligible to sit for the CCDS exam? For those of you who don’t know, the Certified Clinical Documentation Specialist (CCDS) and Certified Clinical Documentation Specialist-Outpatient (CCDS-O) are two credentials offered by ACDIS for those in the profession looking to demonstrate their experience. Neither is an entry-level credential but instead are designed to show excellence and achievement in the field. Those interested in earning the credential must sit for and pass an exam.
Because it is designed for the experienced CDI professional, those wishing to take the CCDS exam must be currently employed as either a concurrent or retrospective clinical documentation integrity specialist and meet one of the following criteria:
- An RN, RHIA, RHIT, MD or DO and two (2) years of experience as a concurrent or retrospective documentation specialist in an inpatient acute care facility using the United States IPPS system.
- An associate degree (or equivalent) in an allied health field (other than what is listed above) and three (3) years of experience as a concurrent or retrospective documentation specialist in an inpatient acute care facility using the U.S. IPPS system. The education component must include completed college-level course work in medical terminology and human anatomy and physiology.
- Formal education (accredited college-level course work) in medical terminology, human anatomy and physiology, and disease process, or the AHIMA CCS or CCS-P credential, and a minimum of three (3) years of experience in the role as a concurrent or retrospective documentation specialist in an inpatient acute care facility using the U.S. IPPS system.
Note that ACDIS defines an inpatient documentation specialist as someone who conducts daily reviews of medical records for patients who are currently hospitalized or treated in the inpatient setting (concurrent) or reviews medical records daily of post discharge, pre-bill records (retrospective).
Both concurrent and retrospective documentation specialists also:
- Work collaboratively using real-time conversation with physicians and medical team members caring for the patient
- Use their clinical knowledge to evaluate how the medical record will translate into coded data, including reviewing provider and other clinical documentation, lab results, diagnostic information, and treatment plans
- Communicate with providers, whether in verbal discussion or by query, for missing, unclear or conflicting documentation
- Educate providers about optimal documentation, identification of disease processes to ensure proper reflection of severity of illness, complexity, and acuity and facilitate accurate coding
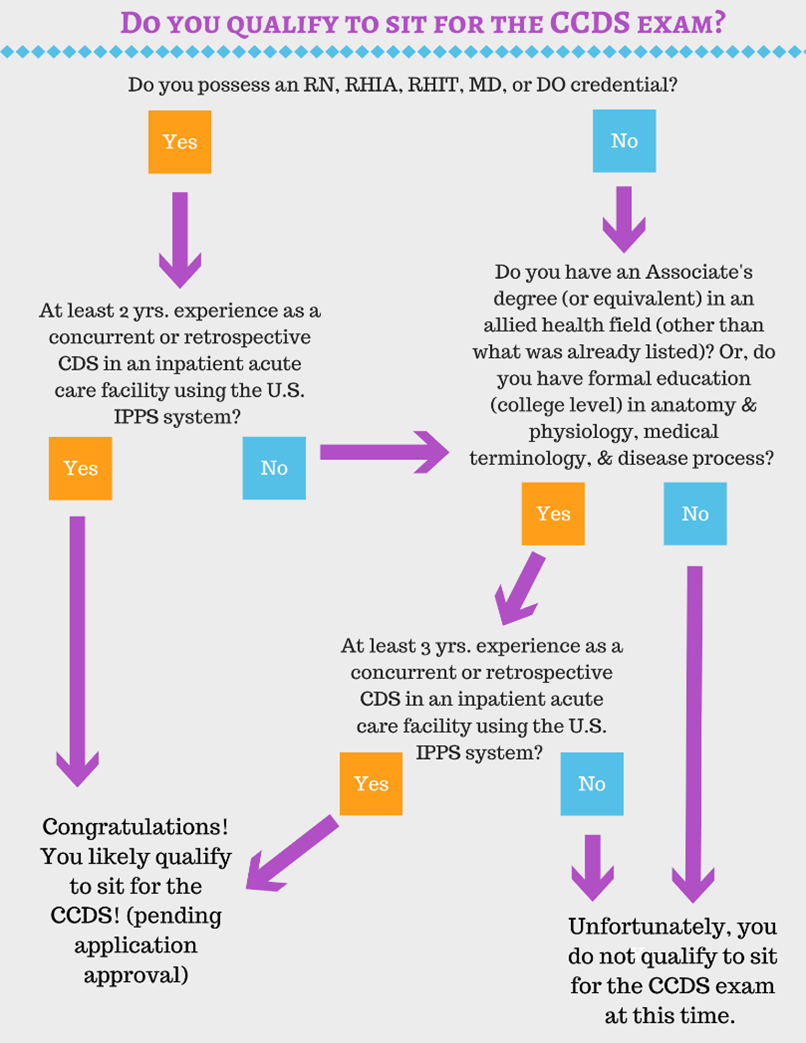
If this sounds like you, you may be eligible to sit for the CCDS exam and can apply here! If you’re still not sure if you qualify, check out our flow chart below for a visual representation of the prerequisites.
Note that eligibility requirements for the CCDS-O differ slightly because it is reserved specifically for outpatient CDI specialists. You can learn more about eligibility for the CCDS-O in our Exam Candidate Handbook, available here.
If you don’t have the requisite experience yet to sit for the CCDS exam, but you still want to distinguish yourself from others, consider becoming an ACDIS CDI Apprentice. The ACDIS CDI Apprenticeship demonstrates that an individual has foundational CDI knowledge and has familiarity with the ACDIS Code of Ethics and other guiding principles for compliant query practice. Individuals who pass the final examination are allowed to use the designation ACDIS-Approved CDI Apprentice on their resumes, biographical information, or email signatures. You can learn more about the apprenticeship here (and its outpatient counterpart here).
As always, if you have any questions or concerns, please reach out to the ACDIS team. We want to see you be as successful as you can be in your role as a CDI professional, and we will do everything we can to help you achieve your goals.
Editor’s note: Accorto is an editor and product coordinator at ACDIS in Middleton, Massachusetts. Contact her at kaccorto@acdis.org.