Radio Recap: CDI past, present, and future
 A lot can change in four years. That’s what the 100th episode of ACDIS Radio focused on. Four years ago, Karen Chase, MS, BSN, RNC, CCDS, now the executive vice president of operations at Accuity Delivery Systems, LLC, in New York, was featured as the very first guest on the new show, back in 2014, discussing her facility’s foray into CDI review for quality measures.
A lot can change in four years. That’s what the 100th episode of ACDIS Radio focused on. Four years ago, Karen Chase, MS, BSN, RNC, CCDS, now the executive vice president of operations at Accuity Delivery Systems, LLC, in New York, was featured as the very first guest on the new show, back in 2014, discussing her facility’s foray into CDI review for quality measures.
At the time, CDI reviews for quality measures were perhaps the foremost new frontier for CDI programs. Now, though, according to Chase, data analytics and the complete clinical picture of each patient has taken its place.
“[In the past] we’ve concentrated on the claims data and the claims data was the one we could max out the reimbursement capacity and then stop adding diagnoses,” she said on the 100th episode of ACDIS Radio, pointing to the once-common focus of CDI programs on CC/MCC capture and DRG optimization. “Now, the reviews are more comprehensive because we have to make sure we show the true clinical picture of that patient in the billing summary.”
That complete clinical picture represented in the billing summary serves a loftier purpose than simple reimbursement, Chase said. “It’s really for population health for the future,” she said. “This data is needed because it’s going to help us improve quality and efficiency of care and help control costs.”
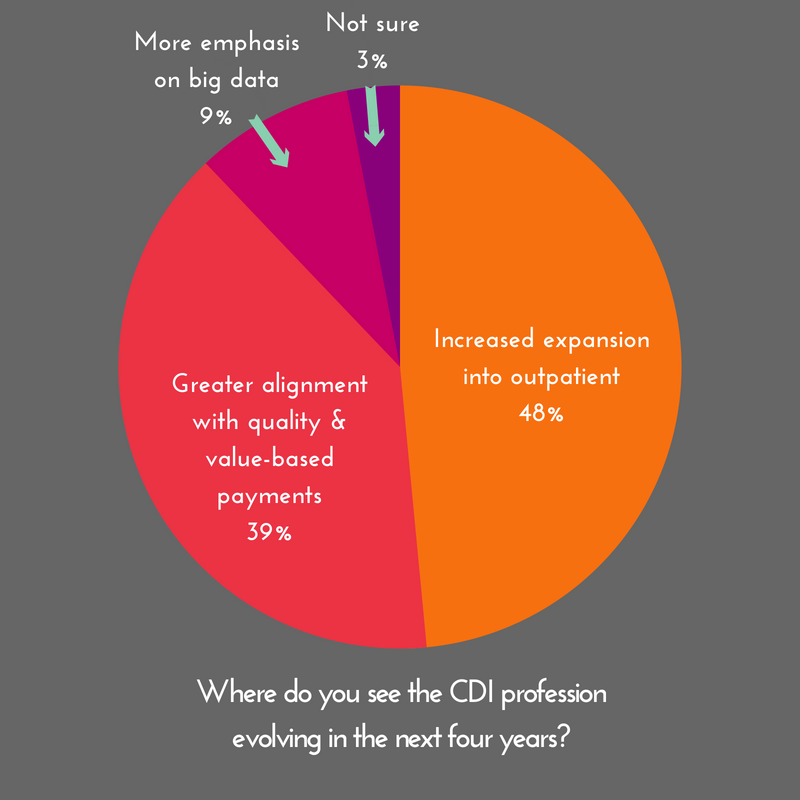
Population health, and the more comprehensive focus of CDI reviews, is now leading CDI programs to expand to other areas of the healthcare continuum. In fact, according to the poll on the episode, 48% of respondents see the CDI profession evolving farther into outpatient settings and services over the next four years.
“Outpatient CDI is a great opportunity and I think it’s something that doctors are going to start paying attention to as they start to realize that their new payment programs will be based on risk,” Chase said.
But, just because it’s a great opportunity doesn’t mean it comes without stumbling blocks. “The biggest challenge or obstacle in this arena right now is going to be the shortage of qualified CDI staff and budget constraints,” Chase said. “Finance departments may want to just layer these reviews onto the existing CDI departments, but I think these are really going to be a different type of review.”
It’s a problem many CDI professionals are well acquainted with, often referred to as mission or scope creep. But, with the differences between inpatient and outpatient CDI, teams may go through some growing pains along the way to expansion.
“I think it’s going to be much more complicated than [leadership] thinks,” said Chase. “I think CFOs are saying, well, you’re looking for CCs and MCCs, now you’re going to look for HCCs. There’s a lot more critical thinking that’s involved with these reviews, though.”
Ultimately, no matter what area CDI expands into, Chase said, it will involve a deeper role with physician education. “I think that CDI has started to take the role of education,” she said. “An hour’s worth of teaching residents is worth a thousand queries.”
Editor’s note: To listen to the complete show from June 27, click here. ACDIS Radio is a free biweekly show. To learn how to register and listen live, click here. To subscribe to the show on Apple Podcasts, click here.
